Clinical and Morphological Features of KidneysÃÆâÃâââ¬Ãââ⢠Damage in Patients with Chronic Hepatitis C
Golubovska O, Herasun B, Kondratiuk L, Nepomnyashchiy V, Bezrodna O, Sukach M and Hrytsko R
Golubovska O1,Herasun B2*,Kondratiuk L1,Nepomnyashchiy V3,Bezrodna O1,Sukach M1 and Hrytsko R2
1Centre for Global Research, RMIT University, Australia
2Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
3State Institution "Institute of Nephrology NAMS of Ukraine", Ukraine
- *Corresponding Author:
- Herasun B
Department of Infectious Diseases
Danylo Halytsky Lviv National Medical University
Lviv, Ukraine
Tel: +38 096 8487785
E-mail: gerab@3g.ua
Received date: February 23, 2016; Accepted date: September 15, 2016; Published date: September 22, 2016
Citation: Golubovska O, Herasun B, Kondratiuk L, et al. Clinical and Morphological Features of Kidneys’ Damage in Patients with Chronic Hepatitis C. J Hep. 2016, 2:2 doi:10.21767/2471-9706.100015
Abstract
The aim of the study was to evaluate frequency, types and renal manifestations in patients with chronic hepatitis C. Our research included 109 patients with chronic hepatitis C. They were examined and treated at the Department of Infectious Diseases of Bogomolets National Medical University and SI "Institute of Nephrology, NAMS of Ukraine." Renal manifestations of chronic hepatitis C were diagnosed in 12.8% of cases. Main clinical and laboratory manifestations included general weakness (was detected in 14 (100%) patients), arterial hypertension (was observed in 11 (78.6%) patients), edema (was observed in 9 (64.3%) patients), proteinuria (was observed in 14 (100%) patients) and microhematuria (was observed in 11 (78.6%) patients), nephrotic syndrome was observed in 9 (64.3%) patients. Arthralgia was observed in 3 (21.4%) patients, and purpura in 1 (7.1%) patient, eGFR reducing was in 9 (64.3%) patients. In 8 (66.7%) patients of our study elevated levels of serum cryoglobulins (from mild to high levels) were detected. According to our data long-term HCV-infection and cirrhosis were considered risk factors for the development of extrahepatic immunological diseases, including renal disease. An important role of renal biopsy in the differential diagnosis and determination of further treatment plan of patients with renal impairment in chronic hepatitis C was pointed out. We noted that kidney damage in patients with chronic hepatitis C in most of the cases were associated with the cryoglobulinemic syndrome. We performed renal biopsies in 12 patients with symptoms of chronic kidney disease and cryoglobulinemic glomerulonephritis was detected in 7 (58.3%) patients. Other types of kidney damage detected in our study included membranoproliferative glomerulonephritis without cryoglobulinemia, membranous nephropathy, focal segmental glomerulosclerosis, mesangioproliferative glomerulonephritis. Keywords: Chronic hepatitis C; Cryoglobulinemic syndrome; Membranoproliferative glomerulonephritis
Introduction
Chronic hepatitis C (CHC) is considered as a systemic disease, with damage of not only the liver, but also with a variety of extrahepatic manifestations. The leading place among them belongs to mixed cryoglobulinemia. Since the discovery of the hepatitis C virus (HCV) in 1988 it has been identified as the main cause of mixed cryoglobulinemia, as it was found in 90% of patients with cryoglobulinemia [1,2]. The classic manifestations of Cryoglobulinemic Syndrome (CGS) is weakness, arthralgia and purpura (Meltzer triad). Other symptoms include damage of other systems such as kidneys, peripheral (less frequently central) nervous system, gastrointestinal tract, lungs, etc. [3,4]. Renal disease in patients with HCV– infection is considered to be a proven fact [5,6]. The most common is Membranoproliferative Glomerulonephritis (MbPGN), which is associated with the II type of cryoglobulinemia (cryoglobulinemic Glomerulonephritis (GN). Less common MbPGN without cryoglobulinemia, Membranous Glomerulonephritis (MGN), Focal Segmental Glomerulosclerosis (FSGS), mesangioproliferative glomerulonephritis, fibrillary glomerulonephritis and imunotaktoid glomerulopathy [7- 17]. There are also other atypical cases of kidneys’ damage in HCV–infection–IgA nephropathy, rapidly progressive glomerulonephritis, thrombotic microangiopathy [18-20]. Isolated cases of albuminuria without kidney damage in HCV infection were also described [16]. In general, the prognosis for HCV–associated glomerulonephritis remains poor, not only because of the progression of kidneys’ disease and development of liver cirrhosis, but also through the high risk of cardiovascular complications
Methods
The study was conducted at the Department of Infectious Diseases of Bogomolets National Medical University and at the Department of Nephrology and Dialysis of SI "Institute of Nephrology of NAMS of Ukraine." We observed 109 patients with CHC. Patient selection criteria was diagnosed chronic hepatitis C, according to the classification of chronic hepatitis, proposed at the International Congress of Gastroenterology (Los Angeles, 1994) [21] which was verified by the identification of specific serological and molecular genetic markers of HCV. CGS was diagnosed according to the recommendations of the European Association for the Study of Liver (EASL, 2012) based on presence in serum of mixed cryoglobulins (CGs), antibodies to HCV, positive rheumatoid factor (RF), reduction of complement C4, morphological (leukocytoclastic vasculitis, infiltration of tissues by monoclonal B-cells) and clinical (purpura, fatigue, arthralgia, MbPGN, peripheral neuropathy) criteria [22].
Clinical examination, general laboratory tests, biochemical tests, serological and molecular genetic studies in dynamics were performed in accredited commercial laboratories.
The cryoglobulins levels were detected using spectrophotometry method by calculating the difference of the optical density of the solution of serum in a buffer (pH=8.6) at 4°C and 37°C [4]. Glomerular filtration rate (GFR) was estimated according to MDRD [23].
Morphological study of renal samples were performed in 12 patients. Presence of clinical and/or laboratory manifestations of chronic kidney disease in patients with chronic hepatitis C for the period of 3 months or longer were the main indications for renal biopsy. Renal samples were obtained by percutaneous needle biopsy of the kidney by a standard technique under the supervision of the ultrasound scanner. We used the methods of light, immunofluorescent and transmission electron microscopy. For light microscopy paraffin sections were stained with hematoxylin and eosin, Masson's trichrome, Congo red, Schiff reagent. Jones silver staining was also used. Direct method of Coons with FITC labeled polyclonal antibodies to IgA, IgG, IgM, and light chains κ and λ, fibrinogen and complement fractions C1q and C3 in dilution 1:10 - 1:60 (DAKO, Denmark) was used on frozen sections of kidneys for the immunofluorescence study. Fluorescence microscope Olympus BX-51 (Japan) was used for the light and immunofluorescence studies. The material for the electron-microscopic study was embedded in EPON-araldit mixture using an ultramicrotome LKB-III (Sweden) for production of semithin and ultrathin sections. Semithin sections were stained with toluidine blue. Ultrathin sections were contrasted with 2% solution of uranil acetate and plumbum citrate and examined with an electron microscope TEM-125K (SELMI, Ukraine) at an accelerating voltage of 60 kV. Morphological diagnosis was based on morphological classification of renal diseases for nephrology practice, 2010 [23].
Statistical analysis of the results was performed by using descriptive statistics. Calculations of the results were performed using the software package "Statistica 6.0".
Results
We observed 109 patients with CHC. Renal lesions were diagnosed in 14 (12.8%) patients. Baseline characteristics of the patients presented in Table 1.
| Age, years | 40,3 ± 12,6 |
| Sex ratio (M/F) | 8/6 |
| Estimated duration of HCV-infection, years | 10,2 ± 3,7 |
| General weakness | 14 |
| Hypertension | 11 |
| Lower extremities and face swelling (edema) | 9 |
| Dry mucous membranes | 2 |
| Arthralgia | 3 |
| Purpura | 1 |
| Dyspeptic syndrome | 2 |
Table 1:.Baseline characteristics of patients with CHC and renal lesions, n=14.
Laboratory tests showed next results: 9 (64.3%) patients were anemic, 7 (50.0%) patients had elevated ESR level, 5 (35.7%) patients had increased creatinine level, 6 (42.9%) patients had increased urea level, 10 (71.4%) patients had hypoproteinemia and hypoalbuminemia, 9 (64.3%) patients had hypercholesterolemia, 9 (64.3%) patients had decreased eGFR. It was noted that hyperbilirubinemia and increased ALT and AST level that indicate the activity of hepatitis were detected only in 3 (21.4%) and 1 (7.1%) patients respectively.
Results of the urinalyses showed that all patients had proteinuria which ranged from 0.24 g/l to 9.5 g/l. Erythrocyturia (from 10 erythrocytes to solid in sight) was observed in 11 (78.6%) patients. Leykocyturia was observed in 9 (64.3%), cylindruria – in 12 (85.7%) patients. Nephrotic syndrome occurred in 9 (64.3%) patients.
Thus, according to the results of clinical and laboratory examination the symptoms of kidney damage in patients with CHC were dominant and the activity of hepatitis was minimal in the majority of these patients. However, it should be emphasized that hepatic fibrosis F3-F4 was detected in 5 (35.7%) patients. Renal needle biopsy with morphological study was performed in 12 patients with chronic kidney disease. In other two patients with transient proteinuria were no indications for biopsy. Cryoglobulinemic GN was diagnosed in 7 of 12 patients (58.3%) according to the results of morphological studies of renal specimens. Two patients had MbPGN without cryoglobulinemia. Membranous nephropathy, FSGS and mesangioproliferative GN was diagnosed in 1 patient respectively.
Increased levels of serum CGs (from mild to high levels) were diagnosed in 8 (66.7%) patients. Seven of these patients had cryoglobulinemic GN and one patient had FSGS.
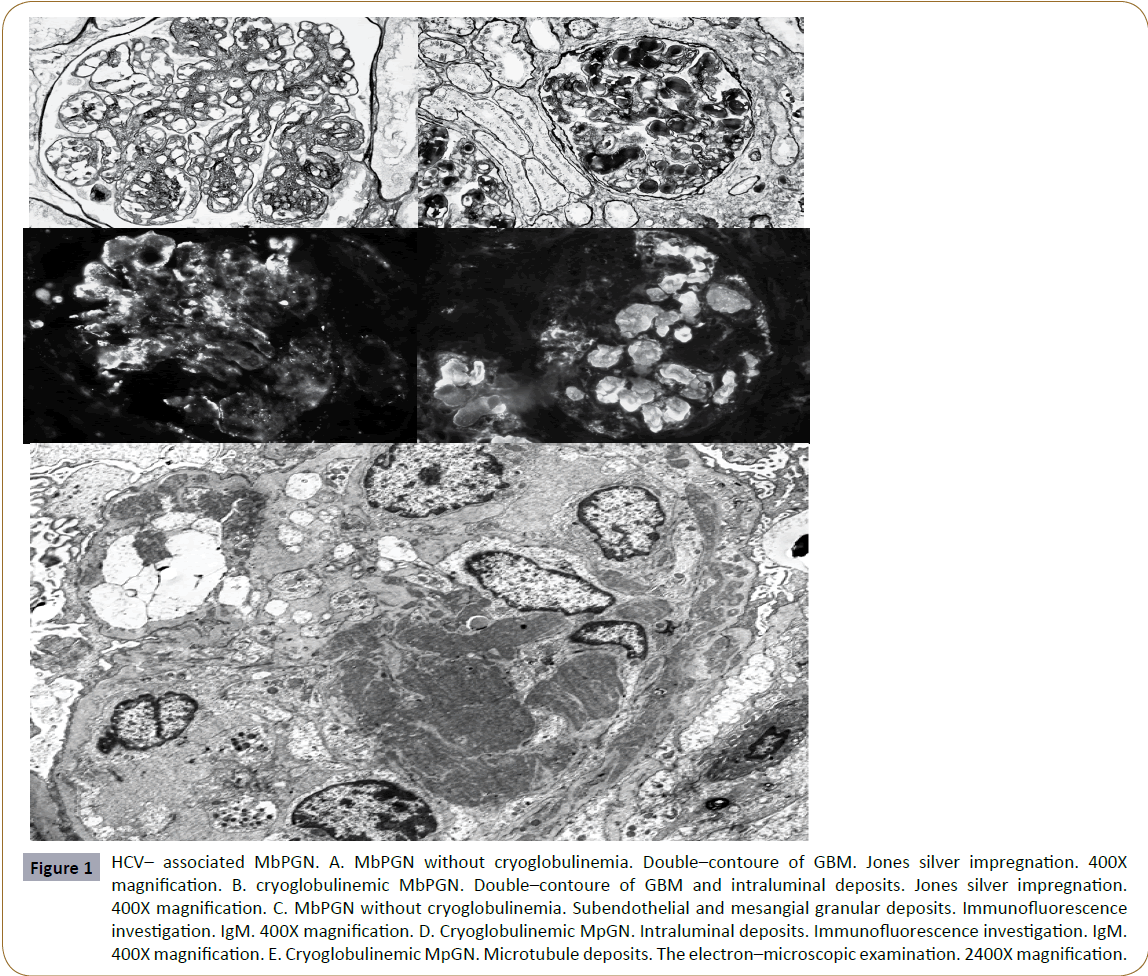
An increased size of the glomeruli with global endocapillary hypercellularity and excess of mesangial matrix was observed in all cases of HCV-associated MbPGN with and without cryoglobulinemia using light and electron microscopic study. Diffuse thickening of the glomerular basement membrane (GBM) was differently expressed in different capillary loops. Thickening parts of GBM at the test samples stained with Schiff reagent and Jones silver impregnation looked like double-contoure (Figure 1a). Infiltration by mononuclear cells of varying degrees of severity were observed in 4 (33.3%) cases. Cellular and fibrouscellular crescents were detected in 2 (16.7%) cases. Numerous subendothelial and mesangial electron-dense deposits were identified using electron-microscopic study. They were small and discrete and also large and elongated. Additional membrane at the pericapillary part was often seen as well as interposition of mesangial cells. Subepithelial electron-dense deposits were observed in 2 (16.7%) cases. The fusion of small processes of podocytes was noted as a characteristic feature.
Figure 1: HCV– associated MbPGN. A. MbPGN without cryoglobulinemia. Double–contoure of GBM. Jones silver impregnation. 400X magnification. B. cryoglobulinemic MbPGN. Double–contoure of GBM and intraluminal deposits. Jones silver impregnation. 400X magnification. C. MbPGN without cryoglobulinemia. Subendothelial and mesangial granular deposits. Immunofluorescence investigation. IgM. 400X magnification. D. Cryoglobulinemic MpGN. Intraluminal deposits. Immunofluorescence investigation. IgM. 400X magnification. E. Cryoglobulinemic MpGN. Microtubule deposits. The electron–microscopic examination. 2400X magnification.
The focal tubular atrophy was detected in 6 (50.0%) patients and accumulation of foamy macrophages was found in the interstices of 3 (25.0%) patients. The areas of fibrosis were detected in 5 (41.6%) patients, focal inflammatory infiltration - in 7 (58.3%) patients. 2 (16.7%) patients had features of myointimal hyperplasia of small arteries.
A characteristic feature of cryoglobulinemic GN was the presence of eosinophilic and PAS-positive hyaline thrombi in the lumen of glomerular capillaries. They were either single (in some capillary loops of the glomeruli) or numerous (in most of the glomerular loops) (Figure 1b). The expressive glomerular mononuclear cells infiltration was also found. Data obtained during electronmicroscopic examination showed the presence of subendothelial, mesangial and intraluminal electron-dense deposits. In some cases it was possible to detect their microtubule or crystalloid structure by high magnification.
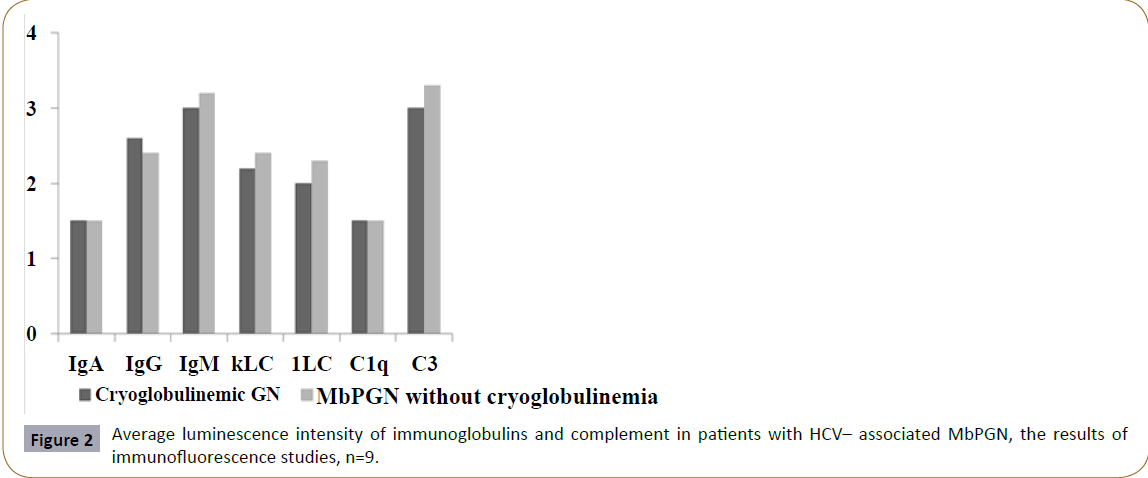
Immunofluorescence investigation in all cases of HCV-associated MbPGN showed small and large granullar deposits of C3, IgM and IgG along the capillary walls and at the mesangium. The highest intensity of luminescence was typical for C3 and IgM (Figures 1c- 1e). Intraluminal deposits in cases of cryoglobulinemic GN were positive for IgM and IgG, as well as for C3. Immunofluorescence investigation data of patients with HCV-associated MbPGN is shown in Figure 2.
Discussion
Renal disease can develop within a few years or even decades after infection with HCV. According to the literature data, the most common form of kidneys’ damage in CHC is cryoglobulinemic MbPGN (PbPGN type I), which is usually associated with type II of cryoglobulinemia [5-10]. Usually MbPGN is diagnosed in patients with long-term HCV-infection. In our study the duration of HCV-infection was 10.2 ± 3.7 years and the average age of the patients was 40.3 ± 12.6 years. According to the literature data MbPGN type I is often diagnosed in patients with HCV-associated liver cirrhosis [24,25]. Hepatic fibrosis F3-F4 was diagnosed in 5 (35.7%) patients in of our research. Thus, long-term HCV-infection and hepatic fibrosis F3-F4 are risk factors for the development of kidney damage in patients with CHC.
Clinical course of the disease in patients with impaired renal function usually include other symptoms of cryoglobulinemia: purpura, arthralgia, fatigue, which were also seen in patients of this study (general weakness – in 14 (100%) patients, arthralgia - in 3 (21.4%) patients, purpura - in 1 (7.1%) patient. According to the literature data, symptoms of kidney damage approximately occur in one third of patients with CGS. Renal symptoms of cryoglobulinemia include nephrotic syndrome, isolated proteinuria (that can be the only symptom of kidney damage in CHC for a long time), microscopic hematuria, 80% of patients develop hypertension [26]. In our study, hypertension was diagnosed in 11 (78.6%) patients, swelling of the lower extremities and face - in 9 (64.3%) patients, proteinuria was found in all patients, microhematuria–in 11 (78.6%) patients. Nephrotic syndrome occurred in 9 (64.3%) patients.
The results of this study also confirm studies of foreign authors: the majority of patients–7 (58.3%)–with chronic hepatitis C and kidney lesions were diagnosed morphologically with cryoglobulinemic GN, the major pathogenetic link of which is the deposition of the CG in the capillaries and glomerular mesangial. However, there were other types of renal injury in this study– MbPGN without cryoglobulinemia (in case of which the deposition of immune complexes (HCV antigens, IG, complement fragments) occurred in the mesangium); MGN (in case of which the subepithelial deposition of immune complexes (antigens of HCV, IG, complement fragments) develops); FSGS (associated with direct damage of podocytes caused by hepatitis C virus) and mesangioproliferative GN (caused by the direct action of the hepatitis C virus on the mesangium through TLR-3 or MMP-2) [27,28].
Conclusions
Thus, our study showed that the renal manifestations of HCV infection appear in 12.8% of cases. The main clinical and laboratory manifestations in patients of our study were general weakness, hypertension, lower extremities and face swelling, proteinuria and microhematuria, nephrotic syndrome and eGFR reduction. We also observed such symptoms as arthralgia and purpura. In our study levels of serum CGs were elevated in 8 (66.7%) patients (from mild to high levels).
The results of our study showed that the long-term HCV-infection and cirrhosis were risk factors for the development of renal lesions.
Needle kidney biopsy is important in the differential diagnosis, since clinical manifestations of kidney damage are usually nonspecific. According to the results of our study, the majority of renal lesions in chronic hepatitis C was linked to the CGS, as cryoglobulinemic GN was found in 7 (58.3%) of 12 patients. There were also other types of kidney damage – a membranous nephropathy, MbPGN without cryoglobulinemia, focal segmental glomerulosclerosis and mesangioproliferative GN.
References
- Golubovska OAInfectious diseases: textbook. Kyiv: Medytsyna; 2012.728 p: Ukrainian.
- Ramos–CasalsM, StoneJH, CidMC, BoschX (2012) The cryoglobulinaemias. Lancet379: 348-360.
- Meltzer M, FranklinEC, EliasK, McCluskey RT, Cooper N(1966) Cryoglobulinemia– – a clinical and laboratory study. II. Cryoglobulins with rheumatoid factor activity. NAm J Med40: 837-856.
- ChopyakVV, Gospodarskyi IIa, HerasunBA (2006) Clinical algorythm of providing medical aid to patients with polyclonic (mixed) cryoglobulinemic syndrome – D 89.1. – Methodological guide of Ministry of Health of Ukraine 33.
- Fabrizi F (2012) Hepatitis C virus, cryoglobulinemia, and kidney: novel evidence Scientifica (Cairo).
- CampiseM, Tarantino A (1999) Glomerulonephritis in mixed cryoglobulinaemia: what treatment?Nephrol Dial Transplant14:281-283.
- D’Amico G (1998) Renal involvement in hepatitis C infection: cryoglobulinemic glomerulonephritis. Kidney Int54: 650.
- MoralesJ, MoralesE, AndrèsA, PragaM (1999) Glomerulonephritis associated with hepatitis C virus infection. Curr Opin Nephrol Hypertens8: 205.
- CosioFG, RocheZ, AgarwalA,Falkenhain ME, Sedmak DD,et al. (1996) Prevalence of hepatitis C in patients with idiopathic glomerulopathies in native and transplant kidneys. Am J Kidney Dis28:752-758.
- AltraifIH, AbdullaAS, al SebayelMI (1995) Hepatitis C associated glomerulonephritis. Am J Nephrol 15: 407- 410.
- Stehman-Breen C, AlpersCE, FleetWP, JohnsonRJ (1999) Focal segmental glomerular sclerosis among patients infected with hepatitis C virus. Nephron81: 37-40.
- Horikoshi S, Okada T, Shirato I, Inokuchi S, Ohmuro H (1993) Diffuse proliferative glomerulonephritis with hepatitis C virus– like particles in paramesangial dense deposits in a patient with chronic hepatitis C virus hepatitis.Nephron 64: 462-464.
- Johnson RJ, GretchDR, Couser WG, Alpers CE, Wilson J,et al. (1994)Hepatitis C virus– associated glomerulonephritis. Effect of alpha– interferon therapy. Kidney Int46: 1700-1704.
- CoroneosE, TruongL,Olivero J (1997) Fibrillary glomerulonephritis associated with hepatitis C viral infection. Am J Kidney Dis29: 132-135.
- MarkowitzGS, ChengJT, ColvinRB, Trebbin WM, D'Agati VD, et al. (1998) Hepatitis C viral infection is associated with fibrillary glomerulonephritis and immunotactoidglomerulopathy. J Am Soc Nephrol9: 2244-2252.
- Latt N, Alachkar N, Gurakar A (2012) Hepatitis C virus and its renal manifestations: a review and update. Gastroenterol Hepatol (N Y) 8: 434-445.
- GerasunBA, ZinchukON, GerasunOB, HrytskoRY (2012) Rheumatologic aspects of hepatitis B and C.Gepatologia 3: 13-23.
- GonzaloA, NavarroJ, Barcena R,Quereda C, Ortuño J (1995) IgA nephropathy associated with hepatitis C virus infection. Nephron N 69:354.
- HerzenbergAM, Telford JJ, De LucaLG, Holden JK, Magil AB (1998) Thrombotic microangiopathy associated with cryoglobulinemicmembranoproliferative glomerulonephritis and hepatitis C. Am J Kidney Dis 31:521.
- UsalanC, ErdemY, Altun B (1998) Rapidly progressive glomerulonephritis associated with hepatitis C virus infection. Clin Nephrol49: 129-131.
- Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ (1994)Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology 19: 1513-1520.
- Mauss S, Berg T , Rockstroh J, Wedemeyer H (2012) Short Guide to Hepatitis C. Flying Publisher p: 150.
- KolesnikMO(2010) Classification of Diseases of the urinary system and morphological classification of renal disease for nephrological practice. Ukrainian Journal of Nephrology and Dialysis 26: 3-60.
- McGuire BM, Julian BA (2006) Glomerulonephritis in patients with hepatitis C cirrhosis undergoing liver transplantation. Ann Intern Med 144: 735-741.
- Kamar N, Rostaing L, Alric L (2006) Treatment of hepatitis C virus related glomerulonephritis. Kidney Int 69: 436-439.
- Prabhakar S (2011) Update on Glomerulopathies – Clinical and Treatment Aspectsp: 468.
- Fabrizi F, PlaisierE, SaadounD, Martin P, Messa P,et al. (2013) Hepatitis C virus infection, mixed cryoglobulinemia, and kidney disease. Am J Kidney Dis61: 623-637.
- AkiraS,TakedaK,KaishoT(2001) Toll–like receptors: critical proteins linking innate and acquired immunity.Nat Immunol2: 675-680.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences